
Published by BusinessToday & AstroAwani, image by BusinessToday.
The nutrition transition, often overlooked, remains a complex and multifaceted global epidemic that is also gaining traction in Malaysia.
The term “nutrition transition” describes the shift from conventional dietary habits towards foods that are often high in sugar, saturated fats, and calories such as fast foods, ready-to-eat meals, processed and ultra-processed foods, etc. This shift in diet often occurs alongside developments in socioeconomic, demographic, and epidemiological conditions within a community or state.
The World Health Organization (WHO) revealed in 2017 that 3.9 million deaths worldwide were linked to an insufficient intake of fruits and vegetables, directly linked to unhealthy eating habits.
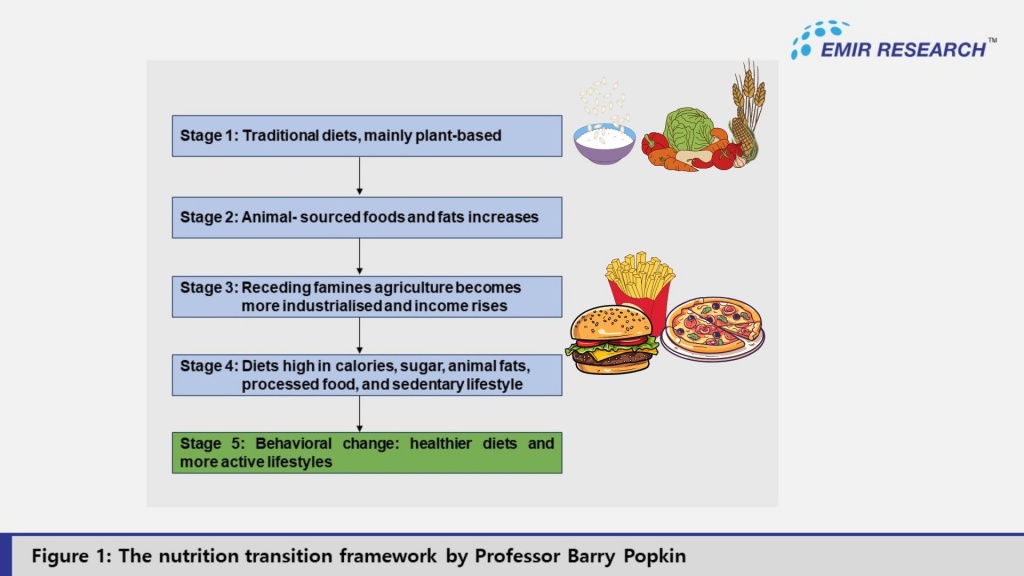
Professor Barry Popkin’s theory (Figure 1) elucidates that these nutritional changes coincide with economic growth. He emphasises that each stage brings health challenges, including obesity and non-communicable diseases, urging interventions to promote healthier dietary patterns and mitigate the negative impacts of nutrition transition.
Socioeconomic Drivers of Poor Dietary Choices in Nutrition Transition
As heavily discussed, socioeconomic inequalities, including income, education, housing instability, etc., pose a significant risk for poor dietary choices. Studies suggest that socioeconomically advantaged households are more likely to have a better quality of life than their less affluent counterparts.
Globally, various findings have consistently identified that nutrition transition is typically more prevalent in low- and middle-income countries (LMICs) due to robust economic development, income disparity, and rapid urbanisation, among others.
In the local context, a cross-sectional study conducted by Chee et.al (2022) involving 2,983 low-income (B40) families revealed that 89.5% of the B40 adults did not consume adequate fruits and vegetables daily. Demographically, the same research discovered that most of the population (68.1%) consume sugary beverages at least once a week, with men (71.7%), Malays (70.3%), and Indians (69.9%) having the highest consumption rates.
Consistently, household food insecurity (HFI) is often linked with poverty, unemployment, and limited access to education and healthcare, which can lead to households relying on cheaper, calorie-dense foods with lower nutritional value due to financial constraints and limited access to nutritious food.
Besides, nutritional outcomes and eating habits are greatly influenced by employment and working conditions, especially for low-income or insecure workers and vulnerable groups residing in urban areas.
People in densely populated areas like George Town and the Klang Valley sometimes have limited time or access to healthy eating options due to stressful work environments, tight schedules, and overwork – considering many individuals are now compelled to take on multiple jobs in order to make ends meet.
These conditions may also result in unhealthy eating patterns, which, in turn, lead to a reliance on fast food and a decline in the quality of one’s diet. Inadequate breaks and extended work hours exacerbate the issue, making it even more difficult to eat healthily.
Importantly, factors such as income levels and the escalation of food inflation, stemming from elevated energy costs, crop failures, and sluggish growth in agricultural productivity have contributed to Malaysia’s inflation rate climbing from 1.5 percent to 1.8 percent in February 2024, marking an increase from 129.8 index points to 132.1 compared to the previous year.
The surge in inflation typically results in elevated prices of nutritious foods like fruits and vegetables, disproportionately affecting lower-income households.
Additionally, the unpredictable climate conditions in Malaysia, exacerbated by the El Niño phenomenon, further restrict access to nutritious foods for these households due to factors such as affordability and availability.
A recent poll conducted by the UCSI Poll Research Center found that among 977 respondents, 492 (42%) reported having financial difficulties when purchasing food, while the remaining respondents did not face such challenges. Of these 492 respondents, 46% did not have access to a nutrient-dense diet, 35% relied on financial assistance from acquaintances, and 20% skipped meals to get by.
Understanding the Health Consequences of Nutrition Transition
The consumption of these highly energy-dense diets is associated with an elevated susceptibility to diet-related non-communicable diseases (NCDs) such as obesity, type 2 diabetes, cardiovascular diseases, hypertension, and others.
NCDs, as estimated by the World Health Organization (WHO), collectively account for 74% of global fatalities. Alarmingly, nutrition transition has been linked to an increased incidence of certain cancers, particularly those associated with obesity and poor dietary habits.
In the local context, Deputy Minister of Health Lukanisman Awang Sauni has disclosed that unhealthy dietary practices constitute the primary risk factor for NCDs. He has also emphasized that nearly 50% of Malaysians remain unaware of their NCD status, thereby heightening the risk of complications if left untreated.
Based on the 2019 National Health and Morbidity Survey, it is estimated that at least 1 in 2 Malaysian adults are overweight or obese, 1 in 3 are living with hypertension, and 1 in 5 are living with diabetes.
According to Prof. Dr. Mohammad Tariqur Rahman from the University of Malaya,between 1993 and 2019, the proportion of adult males who are overweight or obese rose from over 30% to over 50%.
Besides, inadequate access to healthy meals undermines individuals’ physical and mental performance, with children also bearing the burden of these consequences. Consuming inadequate nutrition has serious and far-reaching implications for the physical and cognitive development of children, as highlighted by EMIR Research (refer to “ Battle against the unseen enemy of childhood stunting”, 2023), leading to health issues such as stunted growth, gastrointestinal disorders, malnutrition, etc.
The practice of an imbalanced diet also leads to premature death. According to the WHO, more than three-quarters of all NCD deaths, and 86% of the 17 million people who died prematurely, or before reaching 70 years of age, occur in low- and middle-income countries. This has recently become a frequent occurrence in Malaysia, especially in the working-age population, where individuals between the ages of 40s and 50s are dying of cardiovascular diseases. According to the Ministry of Health, in 2017, there were an estimated 20,786 deaths of persons of working age in Malaysia as a result of the three main NCDs: cardiovascular disease (13 023 deaths), cancer (7 291 deaths) and diabetes (471 deaths).
Based on the 2022 MOH annual report, the life expectancy of an individual at birth has significantly decreased from 76.9 in 2012 to 76.4 in 2022. In comparison, neighbouring countries such as Singapore have a life expectancy of 83.2 (2019) and Thailand 77.7 (2019).
The prevalence of nutrition transition transcends beyond individuals and households and has implications for the nation-state. The growing prevalence of NCDs places an increased strain on the country’s health system and significantly constrains the nation’s creative and productive potential.
NCDs pose a significant burden to the healthcare industry. In 2022, the MOH, in collaboration with the WHO, released a report titled “The Direct Health-care Cost of Non-communicable Diseases in Malaysia”, stating that the direct healthcare costs of the three selected NCD categories (cardiovascular diseases, diabetes, and cancer) were estimated at RM 9.65 billion in 2017.
While raising the sugar tax will be one of the most effective ways to promote a healthy lifestyle in Malaysia, it may not be well received by many. Therefore, EMIR Research recommends the following alternative policies to the relevant stakeholders:
- The Ministry of Domestic Trade and Cost of Living (KPDN) should consider implementing stricter regulations on food marketing and advertising, particularly targeting unhealthy and processed foods. Clear and informative labelling on food products can empower consumers to make informed decisions about their food choices. Similar efforts have been made by the Vietnamese government in labelling nutrition values in products, which specifically include components such as sodium, energy, protein, carbohydrates, and saturated fats.
- Schools should implement, constantly monitor, and strictly enforce policies to ban the sale of heavily processed junk foods such as nuggets, sodas, ice cream and candies in school canteens and within stipulated distances from school premises. The NHMS 2022 survey highlighted that one in three Malaysian teenagers aged 13 to 17 are overweight or obese, one in three consume soft drinks every day, and four out of five don’t eat enough fruits and vegetables.
- Lowering tariff barriers on unprocessed tropical food, such as fruits, vegetables, nuts, poultry, seafood, etc., would make them more affordable and accessible for consumers to purchase, particularly those in vulnerable communities. This initiative will foster the intake of nutrient-dense, locally sourced food while also aiding regional farmers and agricultural output.
- Property developers should consider (or rather, policymakers should think of corresponding regulations/incentives) setting up community gardens and urban agriculture as part of sustainable residential planning and development in urban areas. By allocating space within residential complexes for communal gardens and agricultural plots, residents will be provided with opportunities to engage in food production, recreation, and community-building which also contributes to the creation of vibrant, resilient, and healthy urban communities.
- The reach of “Jelajah Jualan Rahmah,” “Jualan Rahmah Bergerak,” and similar programmes should be broadened into low-income neighbourhoods, especially in urban areas. Residents with low incomes will benefit from access to reasonably priced, fresh produce cultivated locally. Likewise, this initiative supports the livelihoods of local farmers and encourages healthy eating habits.
Moving forward, as a country committed to SDG, Malaysia must prioritise addressing nutrition transition as a key goal for the near future.
In conclusion, an equitable and healthier future for all can be built through the implementation of efficient policies and programmes that promote health equity and address the underlying causes of socioeconomic disadvantage.
All things considered, the transition to a more nutritious diet and increase in NCDs are directly influenced by socioeconomic disparities, exacerbating health inequities globally. Addressing these gaps requires multiple interventions targeting structural, environmental, and social health parameters.
Jachintha Joyce is Research Assistant at EMIR Research, an independent think tank focused on strategic policy recommendations based on rigorous research.

